Introduction
- The T cell repertoire in a healthy adult is shaped by thymic selection (positive and negative), where naive CD4+ and CD8+ T cells can then interact, and be primed, with “foreign” antigen in the secondary lymphoid tissues
- Antigen engagement via the T cell receptor (TCR) then shapes the repertoire of antigen-specific T cells and most likely the functional attributes of the T cell
- Multiple phenotypes of both CD4+ and CD8+ T cells have been identified which have differing functions
- The key to understanding T cell immunity is knowing the types of T cells and how they expand and contract with antigen and how this process is regulated
- In this section we will focus primarily on CD4+ and CD8+ T-cells, which are known to form what is commonly referred to as conventional T-cells since they express an αβ T cell receptor (TCR), and either a CD4 or CD8 co-receptor.
- Under the category of unconventional T-cells, we have γδ T-cells (discussed in detail under module 7) and natural killer (NKT) cells. “NKT cells are known to possess the phenotypic and functional capacities of a conventional T cells, while also exhibiting the cytolytic activity of natural killer cells. NKT cells recognize glycolipids presented in the context of CD1d, and play a role in allergy, autoimmunity, and host defense against cancer and infections.” (Roberts and Girardi, 2008)
Lymphocytes Perform Adaptive Immune Functions
- The cells of the adaptive immune system, in contrast to those of the innate immune system, interact with the environmental agent in a highly discriminative way, i.e., they display specificity, heterogeneity, and memory.
- These functions are primarily carried out by two types of cells that are involved in the recognition of antigen:
- (1) the thymus-dependent or T lymphocytes, which participate in cellular responses against intracellular pathogens, organ transplants, and malignant cells
- (2) the bone marrow or bursal-dependent B lymphocytes, which provide humoral immunity, i.e., antibody-mediated immunity against extracellular pathogens, their toxins, and other environmental substances.
- As outlined in the previous section, a third group of cells is involved in the presentation of antigen to T cells, i.e., APCs, include dendritic cells, macrophages, and B cells (Table 1).
- APCs take up predominantly protein antigens, cut them into peptides, bind the peptides to major histocompatibility complex (MHC) molecules, and display these presented antigens on their cell surface, where they can be recognized and bound by antigen receptors on T lymphocytes.
- T lymphocytes are identified by a surface cluster of differentiation (CD) molecule named CD3 and are comprised of two major groups: the CD4 and CD8 populations
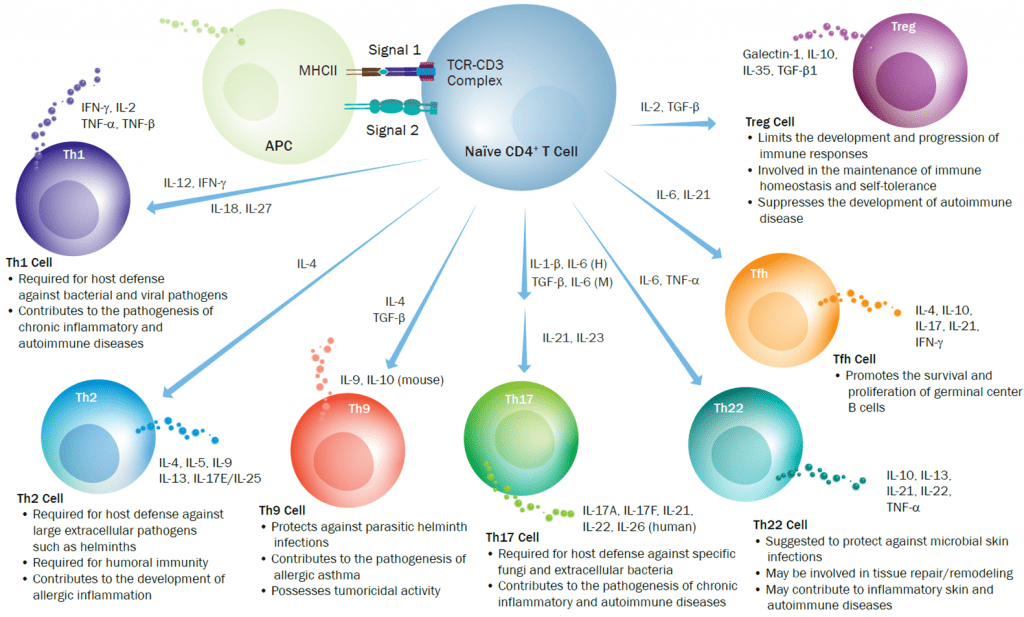
- The CD4 T-cells display helper activities on other populations of cells. Following the onset of T-cell activation naïve CD4+ T cells can differentiate into more specialized subsets such as T helper 1 (Th1), Th2, Th9, Th17, Th22 cells, follicular helper T (Tfh) cells, and regulatory T cells (Tregs) each with a characteristic profile of production cytokines, as shown in Fig 2
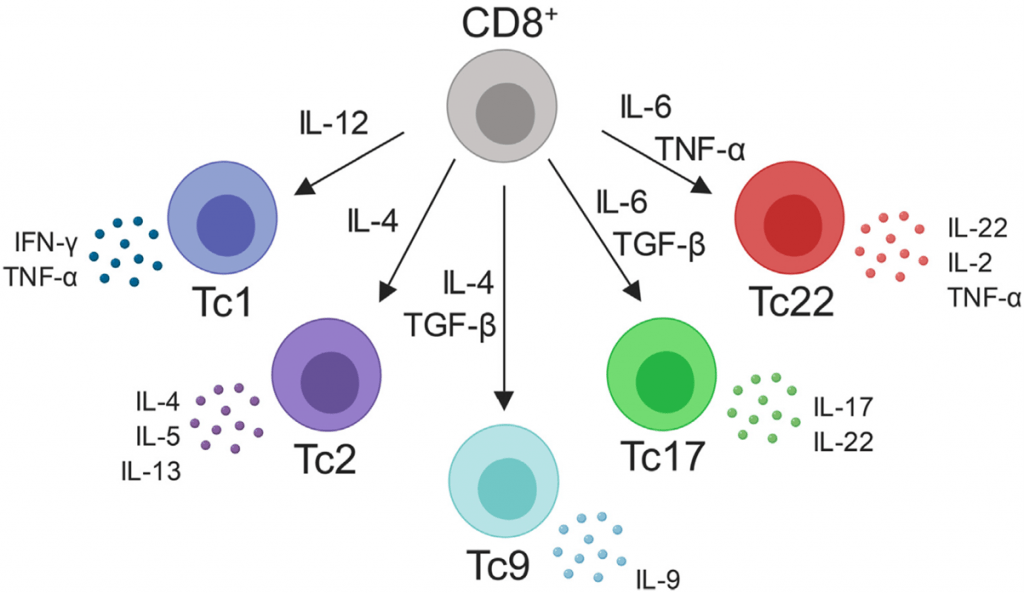
- The CD8 T cytotoxic population is the second major group of T lymphocytes that function in killing target cells; they are comprised of Tc1 and Tc2 subpopulations with similar cytokine profiles as Th1 and Th2 cells. CD8 T-cells were originally taken to be one homogenous population of cells, identified by their production of interferon gamma and protease granzyme B, used to execute their main effector function of killing infected cells (St.Paul and Ohashi,2020). Initially characterized as Tc1 and Tc2 cells, CD8 T-cells are now recognized as having several other subsets (Figure 3) that closely mirror what is seen with CD4+ helper T-cells.
- CD4+ and CD8+ T-cells would form what is commonly referred to as conventional T-cells since they express an αβ T cell receptor (TCR), and either a CD4 or CD8 co-receptor. present in the peripheral blood, lymph nodes, and tissues (such as the skin)
- Collectively, the T lymphocytes play or facilitate a central role in the orchestration of all functions of the adaptive immune system and perform four important tasks:
- (1) promotion of inflammation by cytokine production (Th1 and Th17 cells)
- (2) helping B lymphocytes (Th2 cells)
- (3) regulating immunosuppressive responses (T regulatory cells)
- (4) killing of unwanted target cells (CTL)
Memory T cells
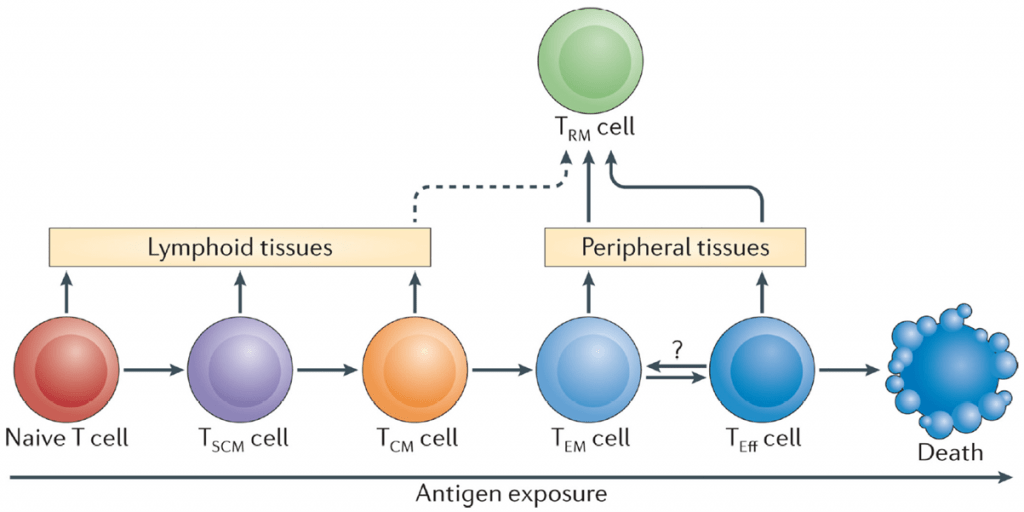
- Effector CD4+ and CD8+ T-cells both have the capacity to give rise to antigen-specific long-lived memory cells T-cells. The characterization and exploration of memory T-cells, has however, been done more extensively in CD8 T-cells.
- The frequency of memory T-cells is known to vary throughout one’s lifetime and has been classified into 3 stages which would include (Farber, Yudanin & Restifo, 2014)
- Memory generation: during the ages of 0-20. This would be the phase where most T-cells are generated
- Memory homeostasis: Taken to occur up to the age of 65 and is hallmarked by a plateau and maintenance in numbers of memory T-cells.
- Immunosenescence: We begin to see differences in the frequency and function of these cells.
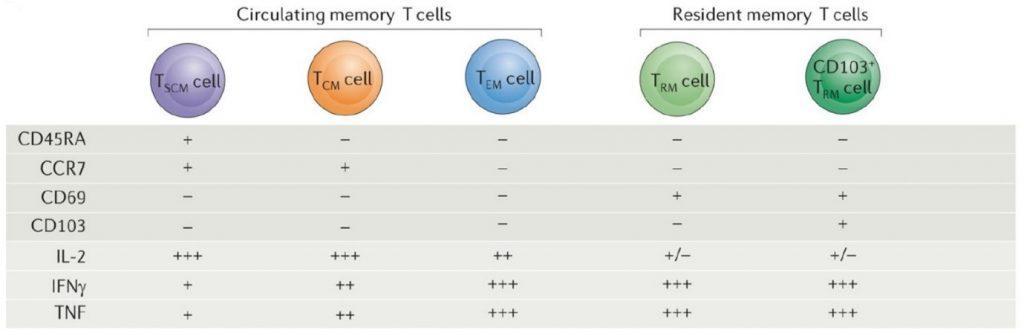
- Depending on the level of antigen exposure, activated naïve T cells can differentiate into various memory T-cells subsets (Figure 4).
- Memory T cells in humans are identified by their expression of the CD45RO isoform and the lack of expression of the CD45RA isoform (CD45RO+CD45RA−) (Farber, Yudanin & Restifo, 2014). Naïve T cells express CCR7, reflecting their primary residence in lymphoid tissue, whereas memory T cells can be divided into CD45RA−CCR7+ central memory T (TCM) cells, which traffic to lymphoid tissues, and CD45RACCR7− effector memory T (TEM) cells, which can migrate to multiple peripheral tissue sites. Figure 5 would show the different markers that can be used to differentiate between these various subsets.
How T cells “see” Antigen
- Because the role of T lymphocytes is to deal with intracellular infections and ‘‘altered self’’ cells (tumor cells), they must have a way to recognize intracellular antigen.
- In addition to their role in innate immunity, dendritic cells and macrophages also play a major collaborative role in the presentation of antigen to T lymphocytes of the adaptive immune system and are therefore referred to as APCs (Table 1).
- Following the uptake and digestion by APCs, foreign substances, usually proteins, are processed by proteolysis into peptide fragments that are later presented to T cells in a highly discriminative manner.
- This process employs cell receptors consisting of molecules on both the surface of the APC membrane (i.e., MHC proteins) (see Chapter 10, Bellanti JA (Ed). Immunology IV: Clinical Applications in Health and Disease. I Care Press, Bethesda, MD, 2012 and the previous section) as well as a specific antigen-binding receptor on the T cell membrane, the TCR
- Of these, the dendritic cells are the most potent APCs, and are particularly important in initiation and promotion of subsequent adaptive immune responses.
- In addition to these cells of the innate immune system, B cells of the adaptive immune system, as described below, can also serve as APCs
Table 1. Various types of antigen-presenting cells
[table id=145 /]
Antigen Processing and Presentation Follows Different Pathways for Cytosolic (Endogenous) and Vesicular (Exogenous) Antigen
- T lymphocytes play a pivotal role in both cell-mediated and humoral immune responses of the adaptive immune system.
- These functions are carried out by T lymphocytes that interact with antigen through the TCR.
- The processing of antigen can occur at two sites: (1) at the level of APCs or (2) at the target cell site.
- Phagocytes and other APCs play major roles in internalizing, processing, and presentation of ‘‘processed antigen’’ to T lymphocytes for induction of immune responses carried out by both CD4 and CD8 lymphocyte populations.
- Antigen can also be processed and presented to T lymphocytes at the target cell site in a cell that has been infected with a virus, for example, or modified by a chemical or by malignant transformation.
- Shown in Figure 1 is a schematic representation of the two modes of antigen processing at these two sites that determines which MHC the processed antigen will react with.
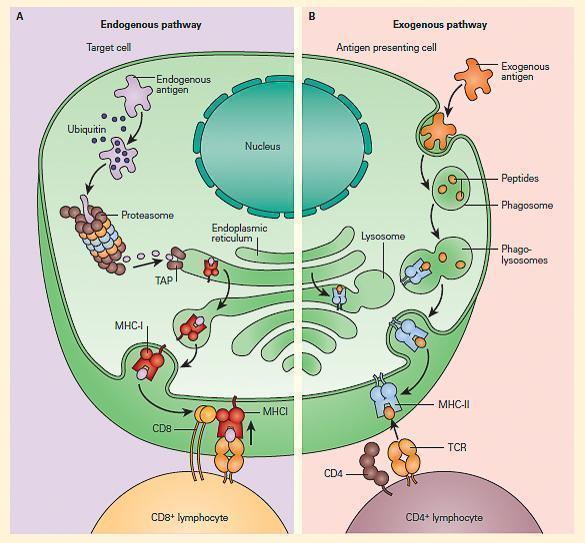
- In the case of antigens processed by APCs by the exogenous pathway, CD4 T cells recognize antigen that has been processed into peptide fragments (epitopes) that are then placed in a groove of the MHC-II molecule, and presented to the TCR on subsets of helper T cells (called CD4+ cells).
- Other antigens found within cells, e.g., target cells, are processed through an endogenous pathway and are delivered by MHC-I to TCR of ‘‘cytotoxic’’ T cells (CD8+ cells).
The Interaction Between APC and T Cells Influences Which T Cells Are Activated
- CD4+ T cell activation results in the secretion of cytokines that help and regulate other cells (see Chapter 9, Bellanti, JA (Ed). Immunology IV: Clinical Applications in Health and Disease. I Care Press, Bethesda, MD, 2012).
- The pattern of cytokine expression defines the subsets of CD4+ T cells: Th1, Th2, Treg1, Th3, and Th17 cells.
- Th1 cells secrete interferon gamma (IFN-y) and create a milieu in which key cytotoxic effectors—macrophages, natural killer cells, and cytotoxic CD8+ T lymphocytes—are activated, generating cell-mediated immunity.
- Th2 cells secrete IL-4 and IL-10 (and other cytokines) and help antigen-primed B lymphocytes differentiate into plasma cells and secrete antibodies, the effector molecules of humoral responses.
- T cells, Treg cells, with the phenotype CD4+CD25+, express the signature transcription factor FOXP3 and usually secrete IL-10 and transforming growth factor beta (TGF-B).
- Cells with this phenotype are thought to recognize self-antigens and function to prevent autoimmunity and are also involved in chronic viral infections, allergy, transplantation, and malignancy.
- Th17 cells represent a wide variety of recently described cells involved in inflammation through the elaboration of proinflammatory cytokines and interact with IL-23 (see Chapter 9, Bellanti, JA (Ed). Immunology IV: Clinical Applications in Health and Disease. I Care Press, Bethesda, MD, 2012).
- As described in the previous section, T cells can recognize peptide fragments that have been processed and presented by APC, i.e., dendritic cells (DC), macrophages, and B cells.
- Figure 2 depicts the shaping of T cell subsets after interacting with antigen and the polarization of T cells in response to different cytokines
- Th1, Th2, Th17, and Treg cells have a variety of interactions with other cells in performing the following functions:
- promotion of inflammation by cytokine production (Th1 lymphocytes);
- helping B lymphocytes (Th2 lymphocytes);
- regulating immunosuppressive responses (Treg lymphocytes).
B cell Interaction with CD4+ T cells
- The antigen primed B cells, expressing antigen-specific BCR’s, interacts with the Th2 CD4+ T cells (in the germinal centres) via MHC-II
- This cognate interaction is critical for B cells to differentiate to plasma cells
Watch video of T cell and B cell interactions
Reproduced with permission from Bellanti, JA (Ed). Immunology IV: Clinical Applications in Health and Disease. I Care Press, Bethesda, MD, 2012.
Th1 Cells Signal Macrophages to Kill Engulfed Intracellular Bacterial Pathogens
- Mycobacterium tuberculosis is an example of a bacterium that can be phagocytosed by macrophages and is able to protect itself from being killed by virtue of its intracellular location within the phagolysosome.
- The organism can now replicate in the phagosome, protected from the harmful effects of the humoral antibody immune response.
- Th1 cells recognize peptides on the macrophage membrane in association with MHC-II, produce cytokines, and signal the macrophage with IFN-g together with other cytokines to kill the bacteria.
- Other Th1 cytokines also attract more macrophages to the infection site and activate them to produce inflammatory cytokines that result in delayed-type hypersensitivity, e.g., the TST.
- One outcome of the host-microbial interaction between the macrophage and the intracellular location of the tubercle bacillus is the killing of the tubercle bacillus resulting from enhanced macrophage killing of the bacillus by activation by IL-12 and later Th1 production of IFN-g
- Or there is failure of killing when the replication of the tubercle bacillus overwhelms the macrophage capacity.
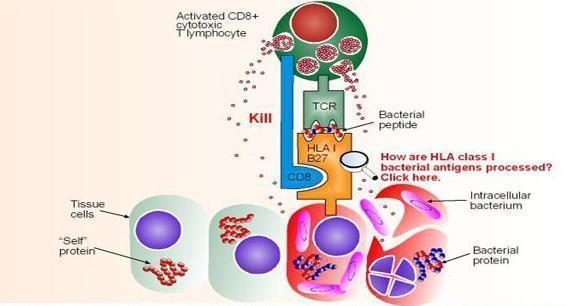
Activated CD8 Cytotoxic T Lymphocytes kill target cells
- Cytotoxic CD8+ T cells effect their function by recognizing peptide bound to MHC-I
- The peptide has been endogenously processed either directly (derived from viral genes, such as HIV) or indirectly, through cross-presentation (derived from effete or dead bacterially infected cells, such as mTB).
- Figure 4 shows activated CD8+ cytotoxic T lymphocytes recognizing a bacterial peptide presented by HLA-B27 (derived from Immunopaedia case study: 14 year old with severe hip pain)
- This causes liberation of cytotoxic granules (perforin and granzymes) from the CD8+ T cell which then cause lysis and apoptosis of infected target cells
Watch a video of the different killing mechanisms, including CD8 CTL
Reproduced with permission from Bellanti, JA (Ed). Immunology IV: Clinical Applications in Health and Disease. I Care Press, Bethesda, MD, 2012.
Quiz
Related Talk
Virginie Rozot, South African TB Vaccine Initiative – T Cell Subsets
References
- Bellanti JA (Ed). Immunology IV: Clinical Applications in Health and Disease. I Care Press, Bethesda, MD, 2012
- Farber, D., Yudanin, N. and Restifo, N., 2013. Human memory T cells: generation, compartmentalization and homeostasis. Nature Reviews Immunology, [online] 14(1), pp.24-35. Available at: <https://www.nature.com/articles/nri3567> [Accessed 28 May 2022].
- Roberts, S. and Girardi, M., n.d. Conventional and Unconventional T Cells. Clinical and Basic Immunodermatology, [online] pp.85-104. Available at: <https://link.springer.com/chapter/10.1007/978-1-84800-165-7_6#:~:text=Unconventional%20T%20cells%20include%20those,that%20arise%20in%20these%20tissues.> [Accessed 28 May 2022]
- Taylor, A.P. The Ever-Expanding T-Cell World: A Primer. The Scientist. August 7, 2017.St. Paul, M. and Ohashi, P., 2020. The Roles of CD8+ T Cell Subsets in Antitumor Immunity. Trends in Cell Biology, [online] 30(9), pp.695-704. Available at: <https://www.cell.com/trends/cell-biology/fulltext/S0962-8924(20)30121-5> [Accessed 28 May 2022].
References
- Bellanti JA (Ed). Immunology IV: Clinical Applications in Health and Disease. I Care Press, Bethesda, MD, 2012
- Farber, D., Yudanin, N. and Restifo, N., 2013. Human memory T cells: generation, compartmentalization and homeostasis. Nature Reviews Immunology, [online] 14(1), pp.24-35. Available at: <https://www.nature.com/articles/nri3567> [Accessed 28 May 2022].
- Roberts, S. and Girardi, M., n.d. Conventional and Unconventional T Cells. Clinical and Basic Immunodermatology, [online] pp.85-104. Available at: <https://link.springer.com/chapter/10.1007/978-1-84800-165-7_6#:~:text=Unconventional%20T%20cells%20include%20those,that%20arise%20in%20these%20tissues.> [Accessed 28 May 2022]
- Taylor, A.P. The Ever-Expanding T-Cell World: A Primer. The Scientist. August 7, 2017.St. Paul, M. and Ohashi, P., 2020. The Roles of CD8+ T Cell Subsets in Antitumor Immunity. Trends in Cell Biology, [online] 30(9), pp.695-704. Available at: <https://www.cell.com/trends/cell-biology/fulltext/S0962-8924(20)30121-5> [Accessed 28 May 2022].