Immunological Memory
Immunological memory can be thought of as the ability of immune cells to interact with a pathogen or microorganism thereby leading to a change in the way the immune system responds to this same pathogen the second time that it encounters it.
The end is just as important as the beginning
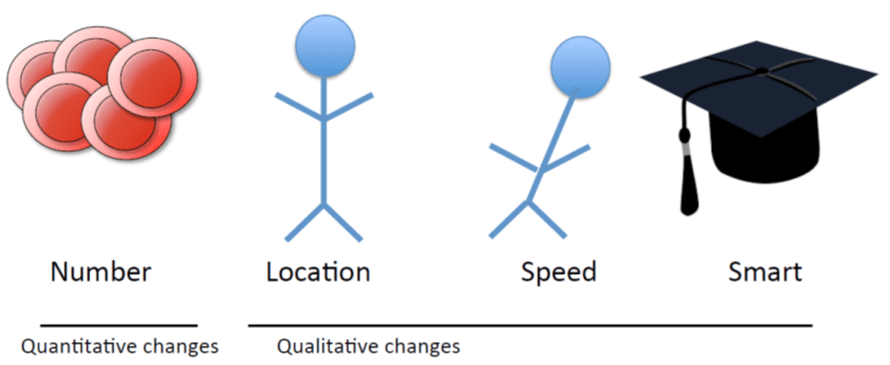
Why are memory responses better than primary responses?
- Altered migration pattern: are poised ready at the site of infection
- Higher affinity: more sensitive, respond to lower levels of infection
- Enhanced effector response
Which cell type can become memory cells?
- Adaptive Immune cells
- Have receptors that specifically recognize microbes
- Innate immune cells
- Have receptors that are activated by microbial products
B cells and antibodies
The duration of the antibody response can vary:
[table id=256 /]
Table 1: Duration of antibody responses after infection or vaccination
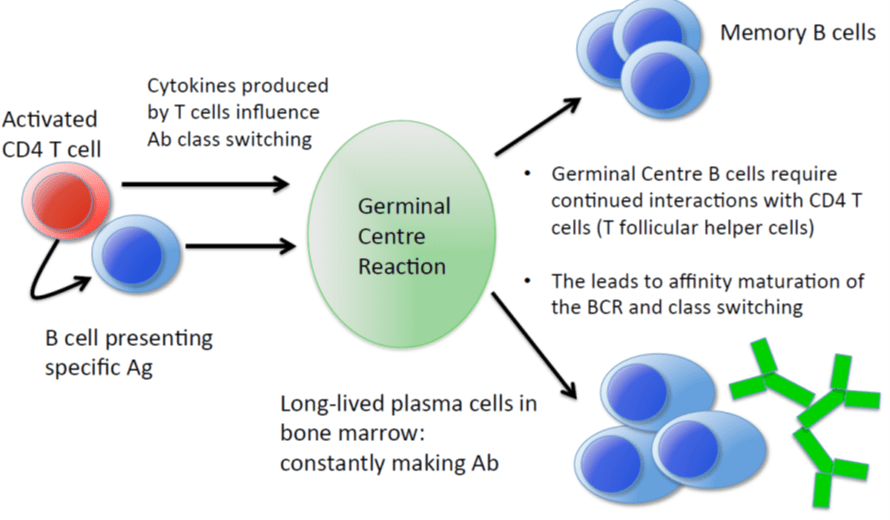
Where does the durable antibody response come from?
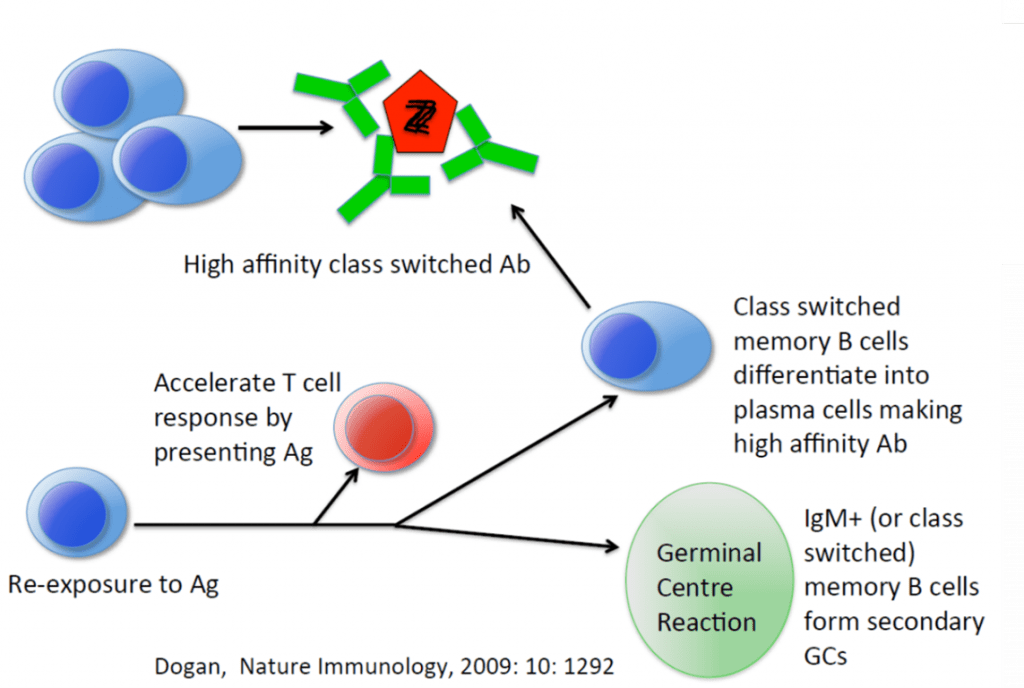
Germinal centers (GCs) are transiently formed structures within B cell zone (follicles) in secondary lymphoid organs – lymph nodes, ileal Peyer’s patches, and the spleen – where mature B cells are activated, proliferate, differentiate, and mutate their antibody genes. GCs play an essential part of where antibody-associated memory is generated.
What signals maintain B cell memory?
- Memory B cells:
- Can recirculate in the blood
- Can be found at mucosal sites (IgA+)
- Can be found at inflamed tissue (IgG2a+)
- Do not require specific Ag to survive but do require a tonic BCR signal
- Long-lived plasma cells:
- Found in the bone marrow
- Found in specific niches that provide survival factors
- For survival require the soluble molecules (APRIL and BAFF) and cell surface molecules (VLA-4 and LFA-1)
How does B cell/Ab memory protect the host?
- Ab can bind and neutralise microorganisms or their toxins
- Opsonise microorganisms to be phagocytosed
- Activate complement
- For example: tetanus, diphtheria, influenza, polio, etc
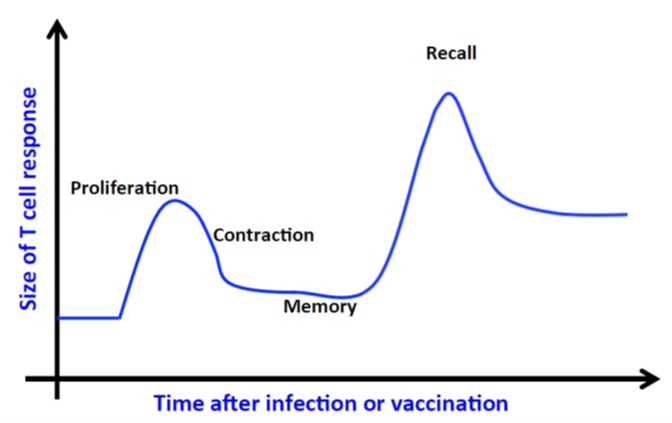
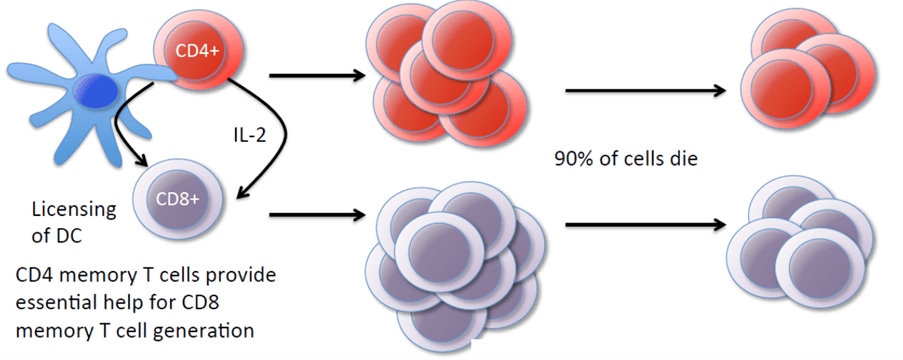
Memory T cell generation
- Activation/Expansion phase
- Mediated by:
- Signal 1: TCR activation
- Signal 2: costimulation (surface molecules)
- Signal 3: inflammatory signals (pro-inflammatory cytokines)
- Mediated by:
- Contraction phase
- Mediated by:
- Cell surface death receptors
- Loss of intracellular survival molecules (Bcl2)
- Mediated by:
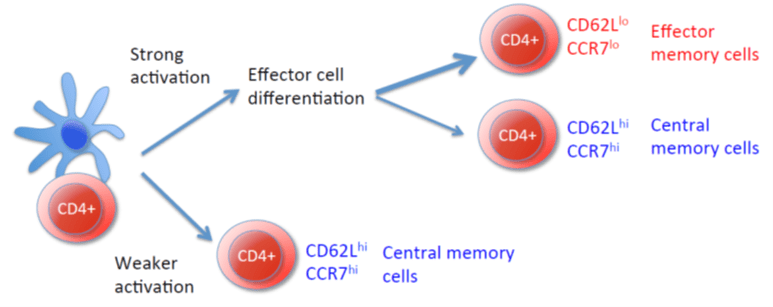
- Memory CD4 T cells can be generated from effector or non-effector T cells
Memory T cells are heterogeneous
- Memory cells undergo periodic homeostatic proliferation but what drives this?
- CD4 memory T cells cannot survive in the absence of IL-7; IL-15 may also provide survival signals
- CD4 memory T cells can survive in the absence of MHC II but are functionally impaired
- CD8 memory T cells cannot survive in the absence of IL-7 or IL-15
- CD8 memory T cells can survive in the absence of MHC I
- Neither CD4 nor CD8 memory T cells require specific antigen to survive
- Persistent antigen can affect the function of the cells (too much leads to exhaustion)
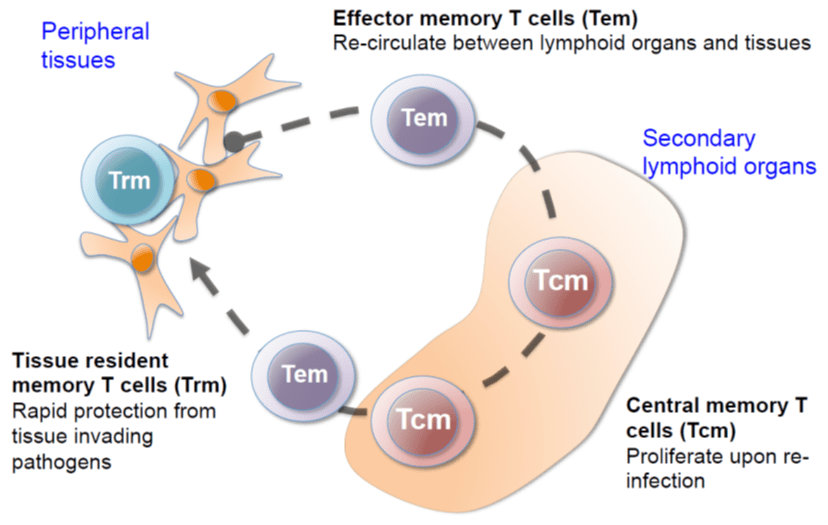
How do CD8 memory T cells provide protection?
- T effector memory cells/ T resident memory cells
- At infection site:
- Kill infected cells via Granzyme B and Perforin
- Make cytokines to activate/attract other immune cells
- T central memory cells
- In lymphoid organs:
- Proliferate rapidly
- Rapidly migrate to areas of infection
- Make cytokines to activate/attract other immune cells
- Self-renew and are multipotent, i.e. can repopulate memory compartment (both Tcm and Tem)
- In lymphoid organs:
- At infection site:
How do CD4 memory T cells provide protection?
- T effector memory cells/Trm
- At infection site:
- Make cytokines to activate/attract other immune cells
- May kill infected cells
- T central memory cells
- In lymphoid organs:
- Proliferate rapidly
- Help B cells to make faster GC response
- In lymphoid organs:
- At infection site:
“Innate memory/Trained immunity”
Immunological memory is taken to be one of the hallmarks of the adaptive immune system. As our understanding of immunology continues to expand, so does the definition and what we know so far about immunological memory. Now, we know that it can also be a characteristic seen in innate immune cells as well. The instances below show us what can result from trained immunity.
- Crustacean, Macrocyclops albidus, can be infected with the tapeworm, Schistocephalus solidus
- Resistance observed if re-exposed to an antigenically similar tapeworm
- The mosquito (Anopheles gambiae) that transmits Plasmodium falciparum demonstrates enhanced immunity following re-infection
- Associated with increased levels of circulating granulocytes
- Mice infected with mouse cytomegalovirus (MCMV) have an expansion of NK cells that express Ly49H
- These cells provide an accelerated protective response upon reactivation
- Humans infected with HCMV have increased levels of NKG2C+ NK cells